PPE Reuse Data: EMS Often Forced to Reuse N-95 Respirators
Of all the changes, adaptions, and extreme circumstances faced by health professionals during the Coronavirus pandemic, one of the more concerning has been the forced reuse of PPE and N95 respirators. After decades of drilling in the concept of one patient, one mask for potential infectious disease calls – EMS agencies were quite suddenly asked to make the best of what they had – including using the same PPE during multiple patient encounters and using equipment beyond the manufacturer’s recommended shelf life and expiration dates.
While this undoubtedly left emergency health care providers with an uneasy sense of compromising patient and provider safety, the disposable equipment’s burn rate was simply too high to remain sustainable. Ambulance agencies around the United States quickly began facing the reality that if they didn’t modify policies, they would soon be facing an extreme shortage of personal protective equipment.
Data on Use and Reuse of N95 Respirators Among All 911 Records
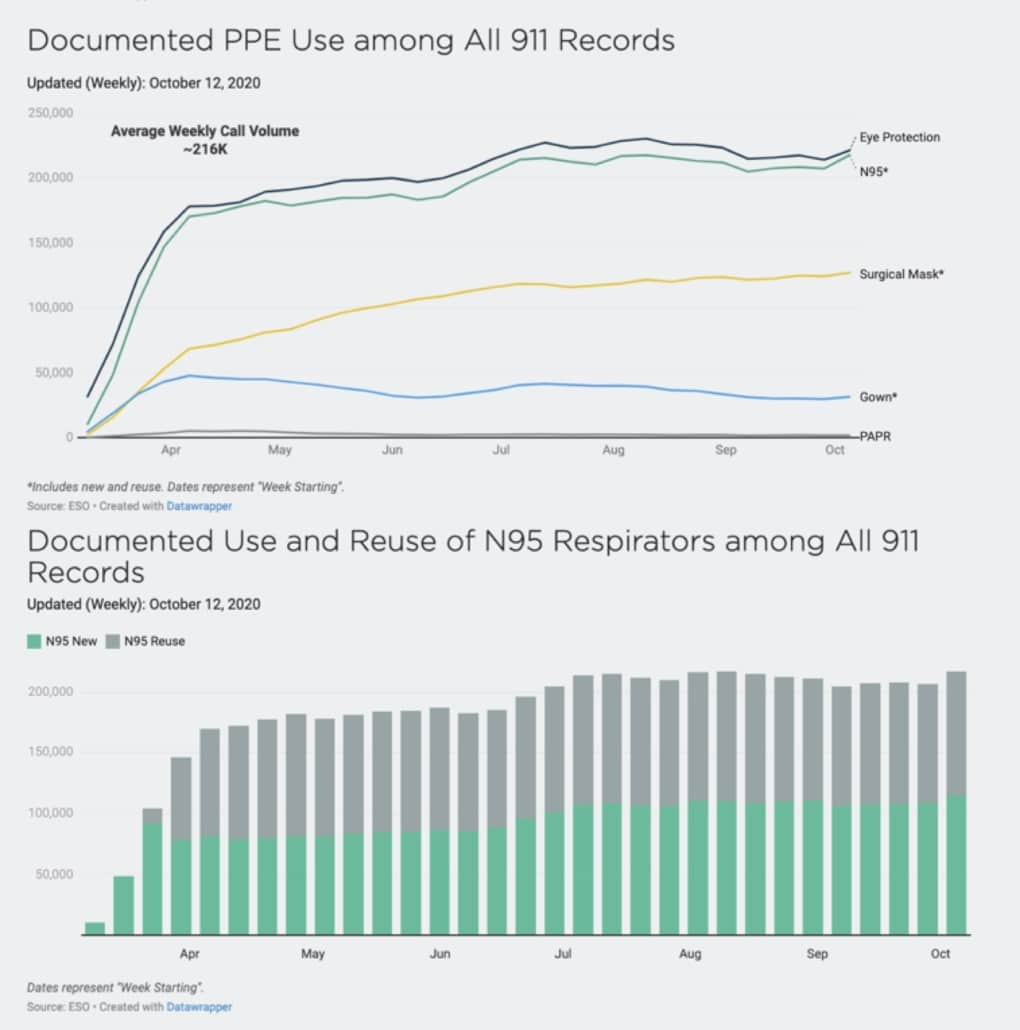
Recently, ESO released the 2020 ESO EMS Index: COVID-19 Special Edition, which reviewed 4.1 million 911 calls from January 1, 2020 – July 31, 2020. This, of course, was the timeframe in which the COVID-19 outbreak began gaining traction in the U.S., and April was a special month that entailed the broadest “stay-at-home” orders/recommendations issued by states.
During the timeframe of this study, data showed that during patient encounters, EMS personnel reported reusing PPE at the following rates:
- Masks: 40% reuse
- Face shield: 41% reuse
- Isolation coverall: 42% reuse
- Gown: 7.4% reuse
Mask reuse (data included any type of mask – N95, N100, P100, or surgical mask) was common, with nearly 50% mask reuse across all 911 responses since April (overall, the data showed approximately a 40% reuse of masks).
Additionally, the reuse rate of PPE steadily increased from the surge in COVID-19 calls, as agencies began to recognize the signs of upcoming supply shortages. For example, in March, the reuse rate of mask reuse was around 13%, but it had jumped to 50% by May. The data also showed a steady decrease in gown usage through June, but then a big jump again in July – consistent with an increase in COVID-19/ILI impressions.
More recent insight into the same database shows that new PPE vs. reuse of PPE rates during the early Fall months remains at around 50%, meaning that agencies continue to attempt to drive down equipment burn rates and employ some new extended use guidelines and discard criteria. Reusing PPE is better than having no PPE, and the possibility of a surge in COVID-19 impressions late in the year continues to present a concern for future supply levels. While many domestic corporations are fast-tracking new manufacturing for PPE, a historical dependency on foreign PPE supply, plus the uncertainty of PPE production as a stable business model, present hurdles in recovering from the shortage, even months after the spike in COVID cases.
Risks of Reusing PPE
While EMS agencies are doing the best with what they have, there is a risk in the reuse of PPE to both providers and patients. New extended use guidelines recommend various cleaning and storing techniques for PPE between patients, but of course, nothing is as safe as donning new PPE with each impression. The exposures to pathogen-laden aerosols from a previous patient and subsequent passing to a new patient are the most prominent concerns. However, health care professionals do their best to clean their PPE thoroughly.
Additionally, new concerns about the chemicals sometimes used to clean PPE equipment – and their heavy use during the pandemic – may be causing additional health concerns for providers. Many products included on the EPA’s list of disinfectants for use against Coronavirus include quaternary ammonium compounds, which release formaldehyde and may be linked to asthma, irritation to skin and eyes, and more severe problems. Many manufacturers are now recommending doing a final wipe-down with a paper towel to remove any chemical residue.
Finally, researchers working to find the best options for disinfecting PPE have found that some disinfectants degrade the mask’s filtration system’s performance. For example, the group found sharp drops in filtration efficiency after two or more treatments with ethanol. Other treatments can degrade the physical structure of the elastic straps or nose clips. However, certain treatments show promising results while reducing the wearer’s risk, such as dry heat, U.V. radiation, and hydrogen peroxide vapor. Their results are still undergoing peer review, but they continue to work for ways to ensure that providers can feel safe reusing PPE during this unprecedented time.
Best Practices for PPE Use
In recognizing the current PPE limitations and availability crisis, the Centers for Disease Control and Prevention began developing and releasing PPE use and reuse guidelines. The first step is for agencies to determine whether they need to employ a “contingency strategy” vs. the more serious “crisis strategy.” The CDC notes that because crisis capacity strategies “are not compatible with U.S. standards of care,” they should only be implemented after conventional and contingency strategies have been implemented.
Additionally, the CDC differentiates use into two categories: “extended use” (wearing the same N95 respirator for repeated close contact encounters with several patients, without removing the respirator between patient encounters) and “reuse” (using the same N95 respirator for multiple encounters with patients but removing – or “doffing” it – after each encounter).
Among the recommendations for extended use, providers should:
- Discard N95 respirators following use during aerosol-generating procedures.
- Discard N95 respirators contaminated with blood, respiratory or nasal secretions, or other bodily fluids from patients.
- Discard N95 respirators following close contact with, or exit from, the care area of any patient co-infected with an infectious disease requiring contact precautions.
- Consider the use of a cleanable face shield (preferred3) over an N95 respirator and/or other steps (e.g., masking patients, use of engineering controls) to reduce surface contamination.
- Perform hand hygiene with soap and water or an alcohol-based hand sanitizer before and after touching or adjusting the respirator.
- Discard any respirator that is obviously damaged or becomes hard to breathe through.
In addition to these guidelines, EMS agencies facing PPE reuse should:
- Hang used respirators in a designated storage area or keep them in a clean, breathable container such as a paper bag between uses. To minimize potential cross-contamination, store respirators so that they do not touch each other, and the person using the respirator is clearly identified. Storage containers should be disposed of or cleaned regularly.
- Clean hands with soap and water or an alcohol-based hand sanitizer before and after touching or adjusting the respirator.
- Avoid touching the inside of the respirator. If inadvertent contact is made with the inside of the respirator, discard the respirator and perform hand hygiene as described above.
- Use a pair of clean (non-sterile) gloves when donning a used N95 respirator and performing a user seal check. Discard gloves after the N95 respirator is donned, and any adjustments are made to ensure the respirator is sitting comfortably on your face with a good seal.
- Follow the manufacturer’s user instructions, including conducting a user seal check.
- Follow the employer’s maximum number of donnings (or up to five if the manufacturer does not provide a recommendation) and recommended inspection procedures.
As the CDC notes, The decision to implement policies that permit extended use or limited reuse of N95 respirators should be made by the professionals who manage the institution’s respiratory protection program, in consultation with their occupational health and infection control departments, with input from the state/local public health departments. The full list of CDC recommendations should be reviewed, and staff thoroughly trained to promote provider safety and ultimately provide better care for the community.
Keeping EMS Teams Safe
Implementing best practices to conserve PPE supply and keep EMS professionals healthy protects EMS agencies and can help with infection prevention and fight the spread of COVID-19. EMS professionals can view more in-depth data on the state of the industry by accessing ESO’s COVID-19 dashboard, including the analytics report on PPE by provider.
Explore more in-depth COVID-19 data for healthcare professionals – updated daily – at the ESO COVID-19 data dashboard.