How EMS Data is Helping Document Emerging COVID-19 Symptoms
As the U.S. continues to wage war on the COVID-19 virus across a wide range of demographic populations, the medical community is beginning to develop a more concrete understanding of the virus’ symptoms and pathology.
However, while the general set of Influenza-like symptoms continues to remain pervasive among patients, there is still much about the virus that researchers are just discovering. Much of this data is being gleaned from EMS impressions and helps evolve best practices for public health regarding PPE, the possibility of airborne transmission, and the effectiveness of masks.
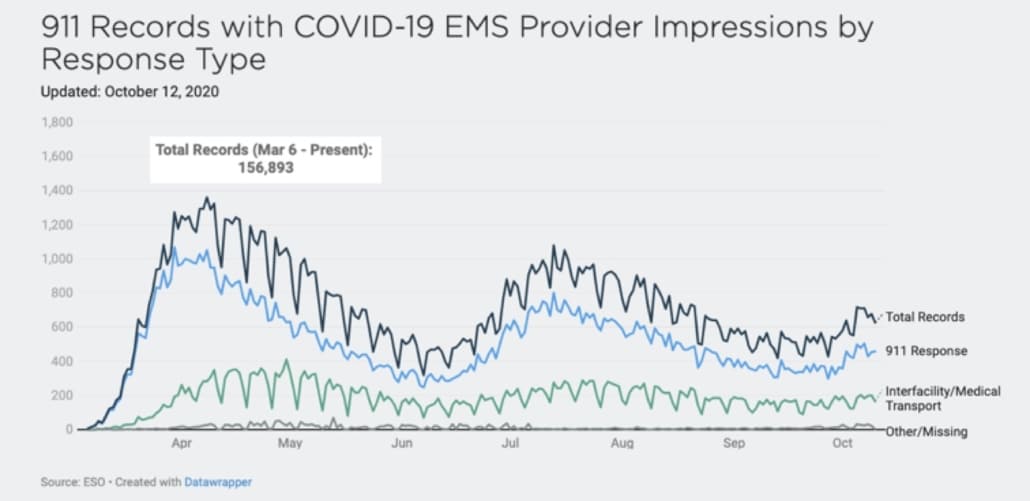
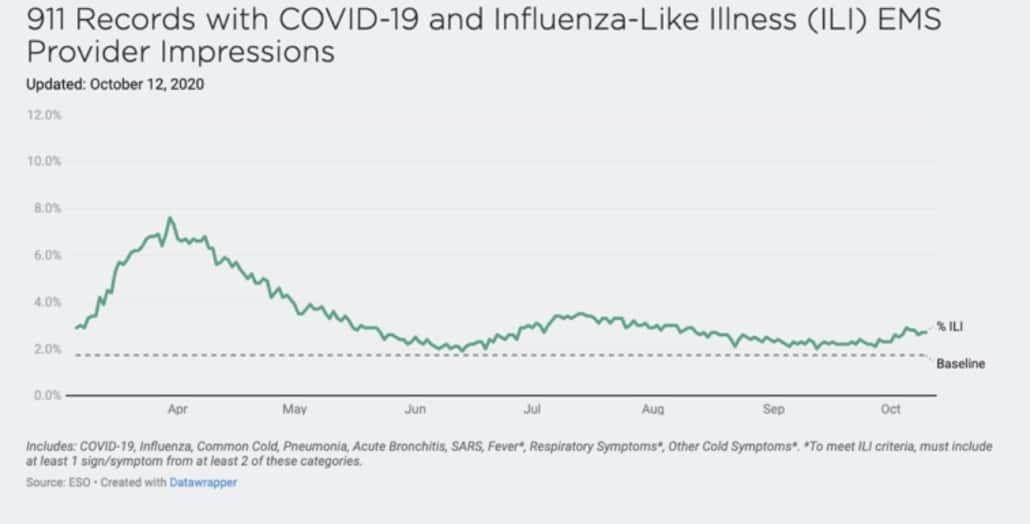
Since March 2020, ESO has maintained several free COVID-19 resources, including a COVID-19 data dashboard based on EMS surveillance data. The online dashboard features a series of snapshot reports and graphs based on data obtained from the ESO database, consisting of more than 2,600 EMS agencies across the U.S., and updated daily. Among the numerous variables tracked on the dashboard, a helpful insight is data on the symptoms of COVID-19, especially among new Coronavirus cases, and how they are different from the seasonal flu.
911 Records with COVID-19 EMS Provider Impressions by Response Type
Symptoms of COVID-19: What the Data is Teaching the Healthcare Community
Most Common Symptoms Seen Among Patients
- Shortness of Breath and Difficulty Breathing
- Sore Throat
- Loss of Taste and Smell
- Body Aches and Muscle Pain
- Chest Pain
Symptoms of Coronavirus Vary from Patient to Patient
A particularly perplexing characteristic of COVID-19 is the wide range of symptoms it presents in patients, even in patients who appear to have contracted it simultaneously or who are in the same family. And even within patients sharing similar demographics, the wide range of symptoms makes it difficult to predict a positive COVID test (making screening measures less effective).
For example, a recent Canadian study of 2,400 children and teens between April 13 and September 30, 2020, found that an upset stomach, loss of taste/smell, fever, and headache were the symptoms most predictive of positive test results. However, more than one-third of pediatric patients who tested positive exhibited no symptoms.
Additionally, among the younger children involved in the study, Influenza-type symptoms such as cough, runny nose, and sore throat were as common, if not more common, in children that tested negative. This suggested that the symptoms traditionally perceived to be connected to Coronavirus – and being used in screening for daycares and schools – might not be effective as initially thought.
In a recent publication from Harvard Medical School, researchers note a wide range of symptoms in adults. While some people infected with COVID-19 have no symptoms, others experience fever, body ache, dry cough, fatigue, chills, headache, sore throat, and appetite loss. Additionally, some patients experience more severe symptoms like high fever, severe cough, shortness of breath, and pneumonia.
Still, others are also experiencing neurological symptoms and gastrointestinal (GI) symptoms that may occur with or without respiratory symptoms and might start before the more well-known symptoms. Specific neurological symptoms include loss of smell and taste, muscle weakness, tingling or numbness in the hands and feet, dizziness, confusion, delirium, seizures, and stroke. Gastrointestinal (GI) symptoms include nausea, vomiting, diarrhea, and abdominal pain or discomfort.
Also concerning is a group of patients calling themselves “long-haulers,” who experience persistent symptoms for weeks and months, including extreme fatigue, headaches, brain fog, sensitivity to light and noise, seizures, and damage to their organs. Many experience post-viral symptoms – while testing negative for new infection – similar to those caused by mononucleosis and myalgic encephalomyelitis/chronic fatigue syndrome.
People Most At-Risk for Contracting COVID-19
While there are numerous cases of young, healthy people suffering from COVID-19, data shows that certain populations are more at risk. Those with underlying health conditions might have more difficulty fighting the symptoms of COVID-19, as explained by Johns Hopkins Medicine.
For example:
- Adults 65 and older: As we age, lung tissue becomes less elastic (making respiratory diseases more difficult to battle), while immune systems also tend to weaken with age. Additionally, older adults are more likely to have other long-term health issues that make them more susceptible.
- People with heart disease: Though COVID-19 most directly affects airways and lungs, a person’s heart must work harder during the infection to drive oxygen to the body’s tissues. This can increase the chances of heart attacks and stroke.
- People with lung disease: Chronic airway and lung diseases can set the stage for a more severe infection because of scarring, inflammation, or lung damage.
- People with diabetes: Poorly controlled blood sugar can make viral diseases more dangerous, possibly because higher blood sugar can create an environment where viruses are likely to thrive. Diabetes also can increase inflammation and weaken the immune system.
Additional Data and Insights on the Novel Coronavirus
Research and analysis continue to develop more insight into the viral load and infectious characteristics of Coronavirus. A recent study released in late November 2020 found that SARS-CoV-2 viral load tends to peak during the first week of illness, meaning COVID-19 patients are most infectious two days before symptom onset until about five days after. The study also revealed an association between older age and more extended infectious periods.
Researchers also found that most individuals who were asymptomatic but tested positive for COVI-19 tended to carry the same viral loads as those who are symptomatic. However, those who were asymptomatic tended to be able to get rid of the virus more quickly. While researchers found viral matter shedding for up to 83 days in the upper respiratory tract, none of the studies detected live COVID-19 virus beyond nine days of symptom onset.
In the U.S., the Centers for Disease Control and Prevention (CDC) continues to advise local health organizations and government bodies on best practices for contact tracing, long-established public health processes aimed at disrupting the chain of transmission (in the past, these practices have been used to slow the spread of AIDS and Ebola). Contact tracers use clear protocols to notify, interview and advise close contacts to patients with confirmed or probable COVID-19.
The recommendations from the CDC for those receiving notification that you have been in close contact with someone confirmed with COVID-19 include:
- Self-quarantine, preferably at home, until 14 days after the last potential exposure, maintain social distance (at least 6 feet) from others at all times and follow all CDC guidance on self-quarantine.
- Self-monitor daily for symptoms. Check and record your temperature twice a day. Thermometers should not be shared.
- Contact a healthcare provider immediately if you:
- Feel feverish or have a temperature of 100.4⁰F or higher.
- Develop a cough or shortness of breath.
- Have persistent pain or pressure in your chest.
- Develop a new confusion.
- Are unable to wake up or stay awake.
- Have bluish lips or face.
- Develop mild symptoms like sore throat, muscle aches, tiredness, or diarrhea.
- Avoid contact with people at higher risk for severe illness (unless they live in the same home and have the same exposure as you).
- Get tested in possible. If test results are positive, you will most likely be assigned a case manager to help alert your close contacts.
- If test results are negative, asymptomatic close contacts should continue to self-quarantine for a full 14 days after last exposure and follow all public health authorities’ recommendations. Symptomatic close contacts should continue to self-quarantine until symptom resolution. A second test and additional medical consultation may be needed if symptoms do not improve.
- If testing is not available, symptomatic close contacts should be advised to self-isolate for 14 days and be managed as a probable case. Self-isolation is recommended for people with possible or confirmed COVID-19 who have mild illness and can recover at home.
What Puts EMS Teams & Healthcare Providers at Risk?
Although front line responders tirelessly and bravely continue to strap on their PPE and head recent study back out to their next potential COVID call, the statistics are not in their favor. In fact, the study found that EMS and firefighters were 15 times more likely to be infected during the first wave of the COVID-19 pandemic compared to the general public.
And, just like other Americans, those with preexisting conditions, especially prior lung health issues, were more likely to suffer a severe infection resulting in admittance to a hospital or death. The study, funded by the FDNY, was conducted after the department experiencing medical leave and sickness that affected 40.7% of the EMS and 34.5% of firefighters.
EMS treating patients in their homes and at trauma sites has little to no opportunity to maintain safe distances from patients and often have to lift, move, and transport their patients, increasing the possibility of mask leaks from movement and increasing respiratory demand from their effort. This is combined with the concerning reality of a dwindling supply for PPE, often forcing first responders to make the hard decision of when and what to reuse.
From ESO’s COVID dashboard, numbers on PPE reuse show the increasing trend of providers reusing protective equipment, pushing equipment beyond its manufactured-recommended guidelines. Recently, ESO released its 2020 ESO EMS Index: COVID-19 Special Edition, which reviewed 4.1 million 911 calls from January 1, 2020 – July 31, 2020.
During the timeframe of this study, data showed that during patient encounters, EMS personnel reported reusing PPE at the following rates:
- Masks: 40% reuse
- Face shield: 41% reuse
- Isolation coverall: 42% reuse
- Gown: 7.4% reuse
While the CDC has issued “contingency” and more serious “crisis” guidelines for agencies facing PPE shortage, there’s no denying that PPE reuse – especially the reuse of N-95 respirators – increases the risk of exposure. This appears to be a new job hazard that EMS and firefighters must shoulder and that agencies and PPE manufacturers are desperately trying to negate.
What Agencies Can do to Preempt the ‘Second Wave’
While the U.S. and its initial COVID-19 patients continue to recover as best they can, first responders and hospitals remain on guard and brace themselves for a “second wave” of cases following the winter holidays. Some agencies are taking proactive measures to be better prepared, such as switching from disposable respirators to new elastomeric respirator masks. While this is a more substantial piece of equipment, the hope is to protect their teams better while also helping lighten the load on the overall PPE supply chain (an agency like FDNY who is making the switch was previously going through more than 600 N95 masks a day).
Additionally, agencies are being encouraged to monitor their crews more actively for signs of burnout and secondary traumatic stress. The American College of Emergency Physicians defines burnout as “feelings of extreme exhaustion and being overwhelmed” and secondary traumatic stress as “stress reactions and symptoms that result from exposure to another individual’s traumatic experiences, rather than from exposure directly to a traumatic event.”
In an already stressful job, these elements may seriously affect providers’ mental health and require intervention, whether it means additional time off or counseling sessions. EMS members are also encouraged to take more breaks from excessive news coverage, take good care of physical health and nutrition, and maintain healthy personal connections with friends and family.
The CDC has also released an extensive online toolkit for fire departments with guidelines and best practices to keep their teams safe and healthy. The site contains basic symptom information and guidelines with what to do if and when you are exposed, as well as PPE care and maintenance guidelines.
COVID-19 Data and Resources
For more COVID-19 data for healthcare professionals, visit the ESO COVID dashboard, updated daily.