Selecting Your Next QI Project: Let the Data Be Your Guide
When it comes to improving the health and safety of our EMS professionals, patients, and communities, we all want to do better. If your EMS agency is like most, there’s likely a long list of improvement opportunities waiting to be tackled. Yet, the limited time and resources dedicated to Quality Improvement (QI) make it necessary to pick and choose which areas get worked on first. So, where should you start?
Putting in some QT – quality time that is – choosing an aim, before embarking on your next QI project, can save resources and ensure you are positioned to make a meaningful impact. Follow these simple steps to learn how to best use your ePCR technology and data to support choosing a QI project.
4 Steps to Get Started with Quality Improvement
1. Identify a measure that matters.
Before you spend time diving into any data, you’re going to need internal support to make sure you get the resources you need to be successful. Gaining support depends directly on how well you focus on an issue that matters to your team. You should be able to clearly articulate the ‘why’ behind targeting a specific area for improvement, without hesitation. Often, this reason involves adhering to a known standard of care that has been shown to positively impact your outcome of interest. Spend some time up front thinking about and even writing down why this project matters to you, your patients, and your organization.
- Example: You know for a fact your agency’s leadership is interested in improving outcomes for patients experiencing heart attacks. Just the other day you heard your boss mention wanting to apply for “Mission: Lifeline EMS” recognition related to quality care for patients experiencing STEMI and acute coronary syndrome (ACS).You know that early identification of STEMI in the field by EMS professionals can have a large impact on how well a patient benefits from treatment. In fact, EMS recognition of STEMI setting and activation of the cath lab reduces the time to diagnosis and reperfusion, increasing the chances that a patient will survive a STEMI and experience less disability. Placement of a 12-L EKG by EMS is a known standard of care that increases the odds of prehospital STEMI recognition and leads to better patient outcomes.
2. Make sure your problem/opportunity occurs frequently enough.
The event in question must occur frequently enough to be able to measure and observe change in a reasonable amount of time. Here’s where looking at your data can help you narrow your focus. What types of patient presentations is your agency encountering most frequently? Which are likely to demonstrate room for improvement? How many of these opportunities for improvement happen in a given day, week, month?
- Example: Stroke care for pediatric patients who have sickle cell anemia may represent an important clinical topic. However, your agency is unlikely to see many of these patients in a given time frame. You’d have to wait months or even years to know whether your actions resulted in an improvement.On the contrary, your service is more likely to encounter a sufficient number of patients who experience STEMI to be able to observe differences resulting from a change you made in a short amount of time.Using data obtained from your local hospitals – which can be automated through bidirectional data sharing software – you see that over the last month, your agency has transported an average of 50 patients who were diagnosed with STEMI.
3. Ensure adequate room for improvement.
Again, the right problem offers room for measuring and observing meaningful change. If you’ve decided to target a particular measure and find that compliance is already above 95%, ask yourself, “Is the juice worth the squeeze?” In other words, does it make sense to spend a great amount of time and resources to improve that already high rate of compliance? Or, would spending time targeting a measure with greater space for improvement likely bring bigger results? Use your data to choose an area that offers real room for improvement.
- Example: You’ve reviewed national performance estimates in resources like the ESO EMS Index regarding 12-L EKG placement for adults experiencing chest pain, but you’re pretty sure your agency does well with patients who have this typical STEMI presentation. In fact, a quick look at your data shows 99% compliance today. However, you know that patients experiencing STEMI often present with other signs and symptoms like syncope, weakness, or abdominal pain. Using your data (which can be easily stored, pulled, and sorted through healthcare analytics software), you dig into each of these three measures and find the following:
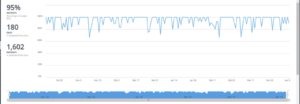
Syncope, 95% compliance:
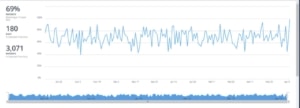
Weakness, 69% compliance:
Abdominal Pain, 32% compliance:
After reviewing the data, you can clearly see that your efforts to detect STEMI among patients with atypical presentations would be best targeted towards improving 12-L EKG placement for patients experiencing weakness or abdominal pain.
4. Refine your project aim.
Looking at your data has provided clear guidance of where to target your limited time and resources to impact something that matters to you, your patients, and your organization; in our example, improved prehospital STEMI recognition. Now, it’s time to get clear about what you hope to accomplish with your project by refining your project aim statement.
- Example: To make the most of your limited resources, you decide to focus on 12-L EKG for the atypical presentation of abdominal pain first. Your aim is to improve 12-L EKG placement for adult patients (ages 35 or older) with an EMS primary or secondary impression of abdominal pain from 32% to at least 60% within the next 6 months.
Finding the right aim to target for QI in a sea of topics begging for attention can be challenging. But rather than fall victim to the pitfall of trying to boil the ocean, doing everything at once, your data can guide your choice of a specific starting point.
Don’t be discouraged if the area you originally set out to improve doesn’t show great promise after looking into your numbers. Examining data and refining your aim multiple times is a normal part of quality improvement. QI projects rarely follow a straight-line path, and in fact, the most successful QI projects involve small, rapid cycles that result in learning, making tweaks, and moving forward again.
By making the most of your data, you can better focus your efforts and help ensure an outcome that is sure to make a difference for your team and your patients.
To learn more about how a well-defined aim statement keeps your QI project from spinning its wheels, read the article, Take Aim to Create Meaningful Process Improvement. And to learn how ESO software can make your data more accessible, check out ESO Electronic Health Record, the next generation of ePCR.