Blog
NEMSIS 3.5: The Important Role it Plays
- Categories :
- Industry Insights
It’s Coming: The New NERIS Standard
- Categories :
- Industry Insights

A Letter From Chris Dillie
- Categories :
- Company Updates

The Fire Service’s Role is Changing.
- Categories :
- Industry Insights
EMS Week 2023: Prioritizing Provider Health
- Categories :

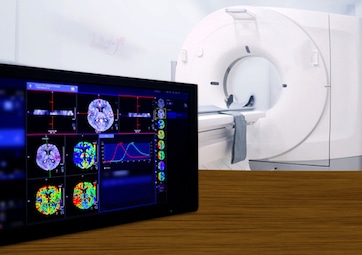
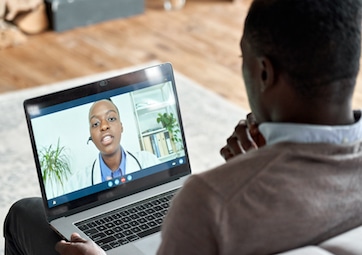
How Telemedicine Is Changing Healthcare
- Categories :
- Industry Insights

Battling Burnout for Nurses
- Categories :
- Industry Insights

What is Mobile Integrated Health?
- Categories :
- Best Practices, Industry Insights

4 Ways to Increase Firefighter Retention
- Categories :
- Company Updates

What is NFIRS?
- Categories :
- Data & Analytics, Industry Insights

Fire Asset Management Explained
- Categories :
- Best Practices, Industry Insights

What is a Fire Preplan?
- Categories :
- Best Practices, Industry Insights

What is NEMSIS?
- Categories :
- Data & Analytics, Industry Insights
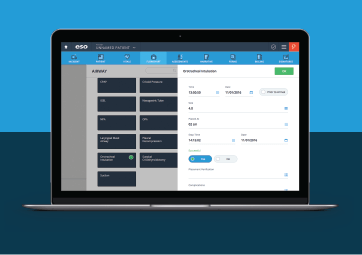
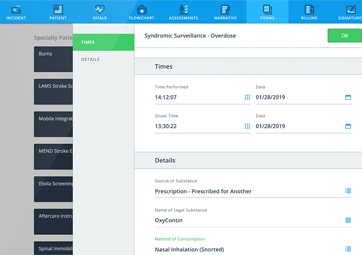
3 Time-Saving Tricks in ESO EHR
- Categories :
- Best Practices, Industry Insights

Unlock Your Fire Data Story
- Categories :
- Best Practices, Data & Analytics
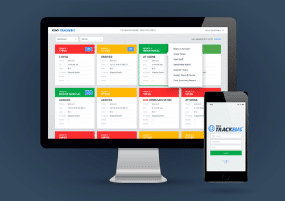
5 Features You Need in a Fire RMS
- Categories :
- Best Practices, Industry Insights
Why You Need Cloud-based Software
- Categories :
- Best Practices, Data & Analytics, Security
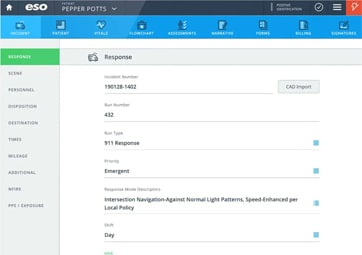
Why You Need an ePCR Integration
- Categories :
- Best Practices, Industry Insights

3 Reasons Fire Preplans Fail
- Categories :
- Company Updates

ET3: What You Need to Know
- Categories :
- Industry Insights

Firefighters’ Silent Killer: Heart Disease
- Categories :
- Best Practices
The History of Columbus FD Engine 18
- Categories :
- Company Updates

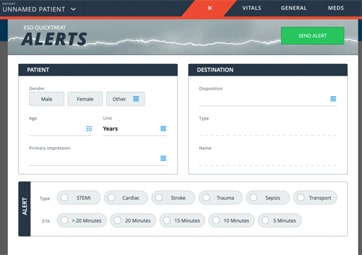
Better Alerting from EMS to Hospitals
- Categories :
- Best Practices
When Hospitals and EMS Share Data
- Categories :
- Interoperability

Let’s Talk Smart Firefighting
- Categories :
- Industry Insights

The Use of Drones in Firefighting
- Categories :
- Industry Insights

A Cheat Sheet for Fire and EMS
- Categories :
- Data & Analytics

EMS Agencies’ Data on the Opioid Crisis
- Categories :
- Data & Analytics
ESO Welcomes New Chief Medical Officer
- Categories :
- Company Updates

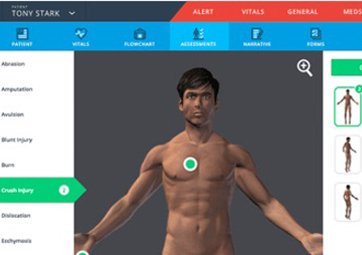
7 Secrets of Smart ePCR Buyers
- Categories :
- Interoperability